Dementia cases are rising rapidly in Northeastern Nigeria, according to new research from the Federal Neuropsychiatric Hospital in Maiduguri, the region’s only specialised mental health facility. The study, which examined data from over two decades, sheds light on the mounting burden of dementia in one of sub-Saharan Africa’s most resource-constrained settings. The findings were published in the journal Alzheimer’s & Dementia.
The analysis reviewed 1,216 patient records of individuals aged 60 and over diagnosed with dementia between 1999 and 2023. Most of the cases (60.5 percent) were attributed to Alzheimer’s disease, followed by vascular dementia at 24.5%. Hypertension emerged as the most common comorbidity, appearing in over 40 percent of patients, while memory loss was the universal symptom across all cases.
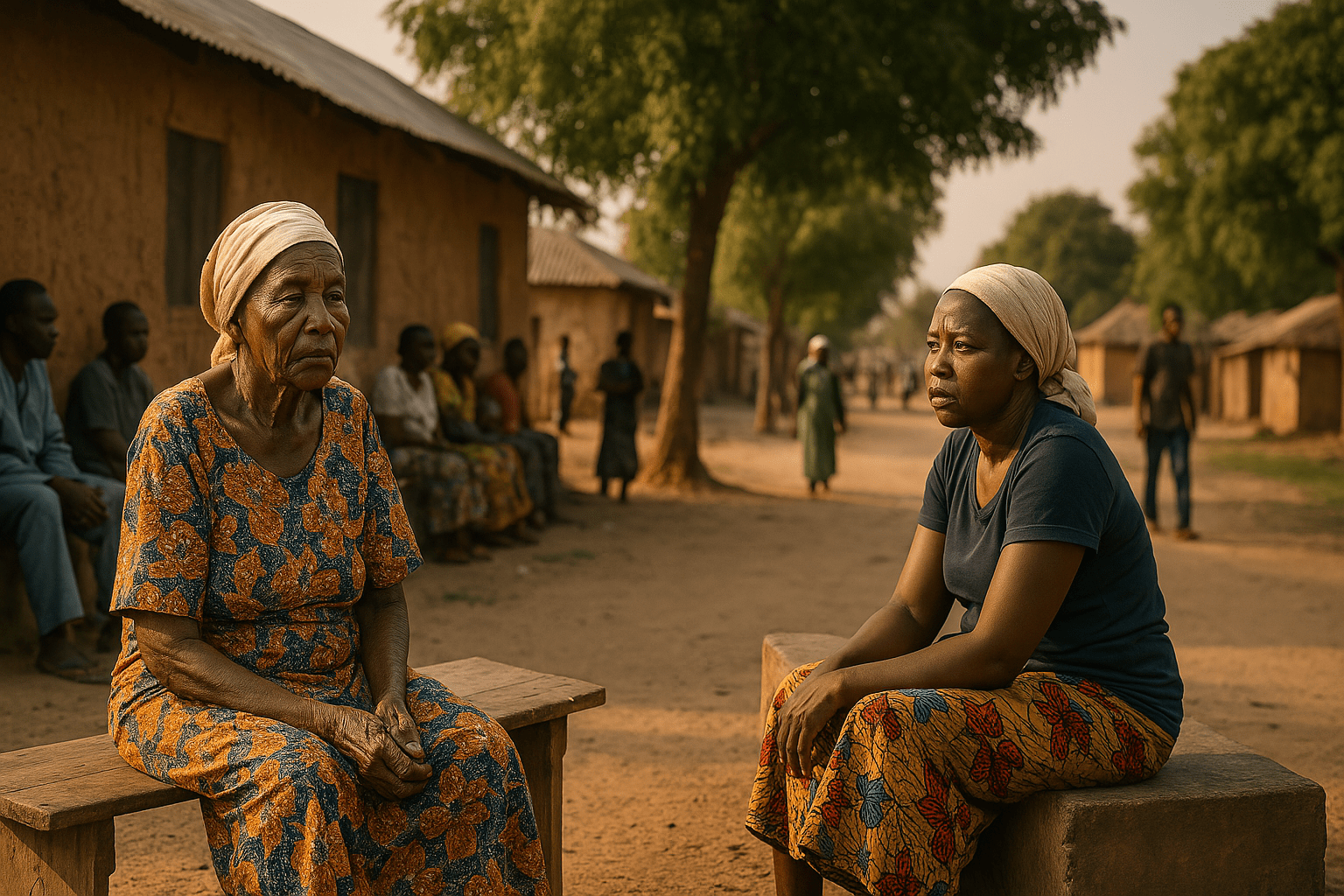
Despite the growing numbers, access to care remains severely limited. The hospital, which serves a population of more than 26 million across six states, is facing challenges in diagnostics, treatment continuity, and infrastructure. In the last five years alone, 423 new cases were recorded, reflecting both an ageing population and an increasing recognition of cognitive disorders. Yet, over 70% of patients failed to return for follow-up care, pointing to a concerning gap in ongoing management.
The study revealed that the majority of patients came from Borno State, particularly urban centres like Maiduguri and Jere. The most affected group were individuals from the lowest socioeconomic class, with nearly 54 percent of patients unemployed. This pattern highlights how poverty and limited education intersect with dementia risk and outcomes.
Cognitive enhancers such as donepezil were administered in more than 80 percent of cases, and supplements like ginkgo biloba were also widely used. However, the range of available treatments was narrow, largely due to financial and logistical constraints. Non-drug therapies, including psychoeducation, were employed in most cases, underscoring the need for holistic approaches in the absence of extensive pharmacological options.
While memory impairment was universally reported, behavioural and neurological symptoms were also observed in a substantial portion of patients. These included agitation, hallucinations, gait disturbances, and confusion, all of which complicate caregiving in settings with limited support services.
Another key finding was the low rate of diagnostic testing. Cognitive assessments like the MMSE were conducted in just over two-thirds of cases, while more advanced investigations, such as neuroimaging or biomarker analysis, were rarely available. The study’s authors noted that this diagnostic gap makes it difficult to differentiate between dementia subtypes or identify underlying causes.
Loss to follow-up was one of the most significant obstacles to care. Cultural perceptions, financial hardship, and the ongoing security crisis in Borno State due to Boko Haram insurgency contribute to low retention in treatment programmes. The doctor-to-patient ratio remains critically low, with an estimated one neurologist for every two million people in Nigeria.
Researchers involved in the project are calling for urgent investment in diagnostic tools, specialist training, and community outreach. The establishment of the Northern Nigeria Dementia Research Group is expected to help fill critical data gaps and inform regionally adapted care models.
As populations age across Africa, the findings serve as a stark warning about the pressures mounting on health systems in under-resourced regions. Without immediate attention, many older adults with dementia risk being left behind.
This article was written by Psychreg News Team from www.psychreg.org
Source link